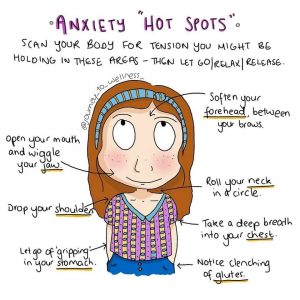
I love this image – it’s a handy way reminder to check in with how we are feeling physically and, possibly, reduce some of our anxiety by acknowledging the physical tension and releasing it, if possible…

Nathalie Griffin, MBACP (Accred), Dip.Sup.
Counselling and Supervision in Bristol
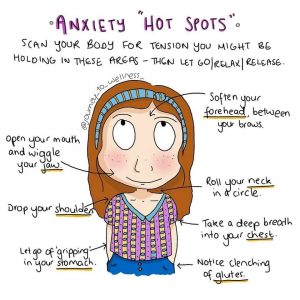
I love this image – it’s a handy way reminder to check in with how we are feeling physically and, possibly, reduce some of our anxiety by acknowledging the physical tension and releasing it, if possible…
Earlier today, I was reminded of Joanna Macey’s Work that Reconnects, specifically The Spiral:
All of us will be able to use different frameworks for reflection and/or problem solving at different times in our lives, and what I like about the Spiral is its simplicity. Starting from a place of gratitude echoes ideas put forth by many therapeutic approaches: Start with identifying the resources we already have and build our resilience by acknowledging and appreciating them. It is important to strengthen our resilience before tackling difficult emotions and/or problems so that we don’t become overwhelmed.
When we’re feeling depressed and anxious, or we’re in a great deal of pain and distress, it can be hard to remember what it is we can be grateful for so I’d like to suggest that it is good mental health hygiene to start a daily gratitude exercise. I have a ‘gratititude jar’ – every morning I write down one thing I am grateful for from the previous day on a small piece of paper, then place it in an old Mason jar, which sits beside my desk. I get a great sense of wellbeing from this exercise, and it gives me more energy to start my day. Conversely, when I struggle to remember what I am grateful for, or I skip the exercise altogether, I take this as a sign that something is amiss and I set aside some time, as soon as possible, to reflect on what is troubling me.
There are many examples of gratitude jars online, but it is simple and cheap: a big enough container to hold a year’s worth of paper slips, scrap paper, a pen or pencil, and a few minutes at some point in the day or night to do the exercise. I find doing it in the morning helps energise me, but it may work better for some people to do it right before bedtime, so you can drift off with a pleasant thought in your mind…
For the third year in a row, my partner and I are off to OffGrid to spend time with people doing great stuff, dance to some great bands, and run some workshops.
We are running two workshops that we did last year, plus a new one about loss, grief, trauma and building resilience.
Here’s a link to our flyer:OG18_3workshops
Here’s a link to the support organisations leaflet we distribute at OffGrid: support_organisations_offgrid2018
Here are the workshop details:
People Care: Three Workshops Building Resilience
(in the struggle for another, better, world)
It’s good to talk! These are faciltated, participatory discussion workshops, not lectures. We live in a crazy & fast changing world, and the often toxic and harmful nature of much social media interaction only serves to heighten our sense of alienation & isolation.
At Off-Grid 2018 we’ll all find a range of activities, experiences & approaches that together offer us a holistic approach to ‘people care’. A key part of that is collective discussion & debate, in a respectful, open & supportive way – tackling issues & life experiences that can derail both our lives and dreams…and finding solutions!
Whilst these three workshops are connected, each one is a stand alone event.
So come along to one, two or all three of the workshops…you choose!
Off-Grid venue – The Nourish Tent
Fri 10th at 2:30 – 4:00pm:
Activist Burnout – what is it & what can we do about it?
We’ll collectively define burnout; sharing our experiences, we’ll identify the signs it’s approaching, and work out ways together to avoid it, or at least lessen its impact!
Sat 11th at 11:30 – 1:00pm:
Activism and Alcohol – a Recipe for Fun, or Disaster?
We’ll look at the pros & cons of alcohol in the activist context; consider who gains most from the relationship between social movements & the alcohol industry; and ask what alternatives there may be? Drinkers, non-drinkers & occassional tiplers all welcome.
Sun 12th at 11:30 – 1:00pm:
Loss, grief, trauma, change and resilience – a discussion
We’ll collectively identify the varied experiences of loss, grief, trauma & change; and consider how we can best cope with and respond to them, to sustain our dreams and struggles for a better life & world.
Please arrive on time!
Because of the potentially personal nature of these discussions, and the flow of the workshop, it can be difficult to integrate latecomers into the workshops.
Content note: references to suicide
With the recent death of Anthony Bourdain, many people took to social media to express their grief. A high profile death can bring people together on social media, expressing support for each other while talking about individual and personal struggles with suicidal thoughts.
It’s also a good reminder to check in on our friends and family, offering to listen to any distress they are experiencing and ask how we can help, while also telling them how much we love them.
However, we need to be careful how we talk about suicide. Whether or not we consider social media to be ‘publishing’ platforms, it can be helpful to keep in mind the Samaritans guidelines on suicide reporting.
In particular, it is useful to be mindful of these points:
“Don’t brush over the complex realities of suicide and its impact on those left behind. Remember that people bereaved by suicide are often vulnerable and are more likely to take their own lives than the general population.”
and
“Speculation about the ‘trigger’ for a suicide, even if provided by a close family member, should be avoided.”
Although the standards of behaviour on social media can leave a lot to be desired, at times of loss and distress, maybe we can all be a bit kinder to each other…
For further support, please have a look at these websites:
I want to highlight this website resource:
https://www.moneyandmentalhealth.org/
Many of the people I work with are experiencing challenges around money.
Sometimes this is because of the increasing difficulties in accessing benefits, or because of a lack of paid work and/or being underpaid at work, or due to pre-existing debt. The people I meet through my work with problem-gambling often tell me that they started gambling in the hope of getting extra money to pay off debts and/or to meet a new financial challenge, liking needing to replace their car. The financial debt that problem-gambling can often create then becomes a trigger in itself to gamble more, in the hope of winning enough money to pay off the gambling debt.
All these situations can be extremely stressful and can feel shaming, so I want to draw people’s attention that there is help and advice out there and encourage people to ask for help. Please have a look at the Money and Mental Health website or Money Saving Expert guide to mental health and debt:
http://images.moneysavingexpert.com/images/documents/mentalhealthguide_new_october_2016.pdf
or ring the National Gambling Helpline: 0808 8020 133 if you are concerned about problem-gambling (yours or that of someone close to you).
I’m currently reading Jenni Murray’s book Is it me, or is it hot in here? A modern woman’s guide to the menopause (Random House, 2003). The writing is ‘light’ while taking the subject very seriously, providing personal stories, helpful tips and medical information.
I’d decided to take Murray’s book out from the library after having increasingly frequent conversations with friends about perimenopausal symptoms, some of which can be quite distressing, and about which many friends seemed slightly embarassed. It got me to thinking about what we feel we can share with friends, even friends of the same age and sex, who we might expect to be more accepting of certain ‘taboo’ subjects. It also got me thinking about how we talk about mental health, as increased levels of anxiety are a frequent event in the build up to the menopause…when does our fear and/or feelings of shame stop us from reaching out to those who we normally trust and love?
All this thinking brought me back to a conclusion (which may sound cliched) I’d reached some time ago: we need to do our best to make space for our loved ones to talk about difficult and scary topics, and also ask our loved ones to make that space for us, because most problems seem bigger and more insurmountable when we feel isolated.
I attended a great PODS training event this past weekend: Working with Dissociative Disorders in Clinical Practice.
Carolyn Spring, the founder of PODS, delivers many of the PODS training events. A survivor of childhood trauma herself, she provides a deep insight into how therapists can engage with trauma and dissociative survivors.
One of the standout moments for me was hearing Carolyn talk about shame-related behaviours: “Shame may keep us alive but it may not keep us safe.” This goes to the core of post-traumatic stress disorder – we all possess effective coping skills to get through traumatic events and the immediate after effects. However, we can then start to live with a heightened senses of threat and self-blame, which get in the way of us acknowledging when we are truly safe and truly unsafe, so we have trouble figuring out how to respond appropriately to our world.
There are many ways to manage post-traumatic stress, and reduce these heightened senses, including one-to-one therapy and practices such as mindfulness.
If you are curious about Dissociative Disorders, including support, please have a look at the PODS website: https://support.pods-online.org.uk/helpline
I was profoundly moved by the Peace Festival in Bristol this week.
Here’s a quick introduction from a University of Bristol press release:
“In August 2017, peace activists from Peru and Colombia gathered in Cartagena de Indias, Colombia, to discuss the ways in which they had used art and creativity to tell stories about the history of conflict in their countries.”
http://www.bris.ac.uk/news/2018/april/peace-festival.html
The film, artwork, and speakers highlighted how important it is to be able to be able to tell our own stories after we have experienced trauma, especially in social and political situations where a dominant narrative might try to silence the survivors. Hence the term ‘memory activist’ – it can be a dangerous and ongoing battle to ensure that the memories and experiences of survivors are heard and, hopefully, justice can be achieved.
I hope to blog here on a regular basis, linking to interesting articles or useful resources, and I’d like to start with something I discovered recently:
The Blurt Foundation
Focussing on depression, Blurt are definitely fighting the battle against the stigma of talking about depression while providing useful resources for anyone living with depression. The Self Care Project book is particularly good…